What is Diabetes?
Diabetes Mellitus is a chronic metabolic disorder characterized by elevated blood glucose levels (hyperglycemia) due to impaired insulin secretion, insulin action, or both.
Types of Diabetes
- Type 1 Diabetes (T1D): Autoimmune destruction of pancreatic beta cells, leading to absolute insulin deficiency.
- Type 2 Diabetes (T2D): A combination of insulin resistance and relative insulin deficiency, often associated with obesity and lifestyle factors.
- Gestational Diabetes Mellitus (GDM): Hyperglycemia first detected during pregnancy.
- Other Types: Includes monogenic diabetes, secondary diabetes due to other diseases or medications, and more.
Pathophysiology
- Type 1 Diabetes: Caused by autoimmune destruction of insulin-producing beta cells in the pancreas. Triggering factors may include genetic predisposition and environmental factors (e.g., viral infections).
- Type 2 Diabetes: Involves a progressive loss of beta-cell function in the context of insulin resistance in tissues like the liver, muscle, and adipose tissue. Chronic inflammation and ectopic fat deposition also play a role.
- Gestational Diabetes Mellitus: Insulin resistance increases naturally during pregnancy, but in GDM, the pancreas fails to compensate with adequate insulin production.
Symptoms of Diabetes
- Polyuria (excessive urination)
- Polydipsia (excessive thirst)
- Polyphagia (excessive hunger)
- Unexplained weight loss (especially in T1D)
- Fatigue
- Blurred vision
Complications
Acute:
- Diabetic ketoacidosis (DKA) in T1D
- Hyperosmolar hyperglycemic state (HHS) in T2D
Chronic:
- Microvascular: Retinopathy, nephropathy, neuropathy
- Macrovascular: Cardiovascular disease, stroke, peripheral arterial disease
- Other: Increased risk of infections, poor wound healing
Diagnosis
Criteria for Diagnosis:
- Fasting Plasma Glucose (FPG) ≥126 mg/dL (7.0 mmol/L)
- 2-Hour Plasma Glucose ≥200 mg/dL (11.1 mmol/L) during an Oral Glucose Tolerance Test (OGTT)
- HbA1c ≥6.5%
- Random Plasma Glucose ≥200 mg/dL in the presence of symptoms
Screening:
Recommended for individuals at high risk (e.g., obesity, family history, sedentary lifestyle) or those over 45 years old.
Management
1. Lifestyle Modifications:
- Diet: Emphasis on whole grains, vegetables, lean protein, and limited refined carbohydrates.
- Physical Activity: At least 150 minutes of moderate aerobic exercise per week.
- Weight Management: Target 5-10% weight loss in T2D for improved glycemic control.
2. Pharmacological Therapy:
- Type 1 Diabetes: Insulin therapy (basal-bolus or continuous insulin infusion).
- Type 2 Diabetes:
- First-line: Metformin
- Additional options: GLP-1 receptor agonists, SGLT2 inhibitors, DPP-4 inhibitors, sulfonylureas, insulin.
- Gestational Diabetes: Insulin is preferred; metformin and glyburide may be used.
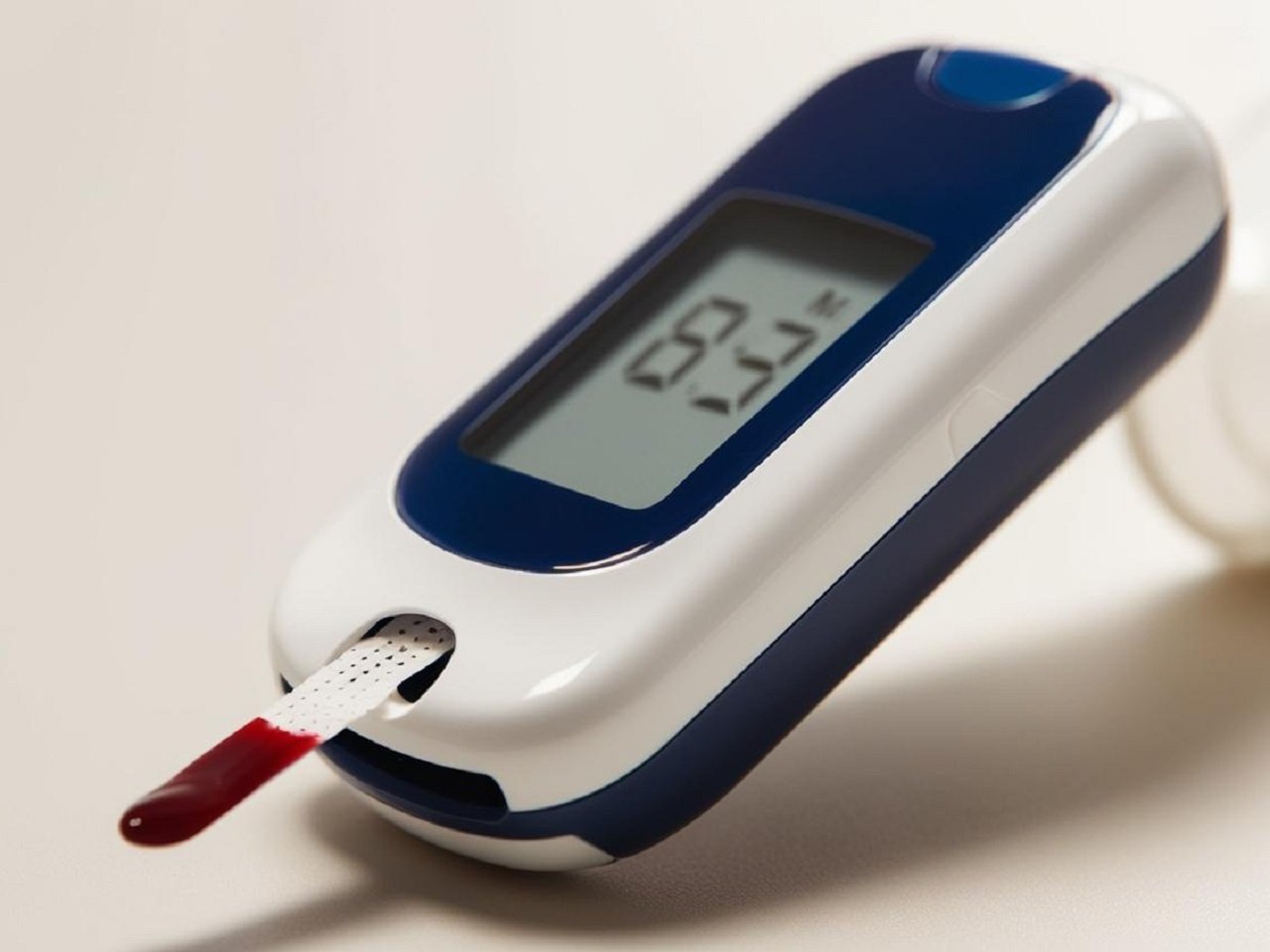
3. Monitoring:
- Self-monitoring of blood glucose (SMBG)
- Continuous glucose monitoring (CGM) for advanced management
- Routine HbA1c testing every 3-6 months
Prevention
1. Type 2 Diabetes:
- Regular physical activity
- Healthy diet
- Weight management
- Early screening for individuals with prediabetes (FPG 100–125 mg/dL or HbA1c 5.7–6.4%)
2. Gestational Diabetes:
- Preconception counselling and optimizing maternal weight
- Regular screening in high-risk pregnancies
Research and Innovations
- Artificial Pancreas: Advances in closed-loop insulin delivery systems.
- Regenerative Medicine: Beta-cell replacement and stem cell therapies.
- Precision Medicine: Genetic profiling to tailor treatments.
- New Drug Classes: Agents targeting novel pathways (e.g., dual GLP-1/GIP agonists).